
Understanding the Crisis
Non-communicable diseases (NCDs) are rapidly increasing, causing over three-quarters of all deaths in many North African countries. In sub-Saharan Africa, where communicable diseases and other health challenges are still prevalent, NCDs such as cancer, cardiovascular diseases and diabetes are increasingly becoming the main cause of mortality in sub-Saharan Africa, where the diseases were responsible for 37% of deaths in 2019, rising from 24% in 2000 largely due to weaknesses in the implementation of critical control measures including prevention, diagnosis and care (6).
NCDs are set to overtake communicable, maternal, neonatal, and nutritional (CMNN) diseases combined as the leading cause of mortality in sub-Saharan Africa by 2030 (2).
In low- and middle-income countries (LMICs), nearly 30% of NCD deaths occur among people under 60, compared to just 13% in high-income countries (4).
Social determinants like poverty, education, housing and socio-economic status impact both communicable and non-communicable diseases. These factors contribute to significant disparities in health outcomes and access to care. Addressing these root causes is essential to improving overall health.
Resource-constrained nations across sub-Saharan Africa and the rest of the global south are now facing an epidemiological transition. They must contend with both communicable diseases and rising NCDs—a dual health burden with significant social and economic implications at all levels.
Lifestyle Factors
Economic growth and global trade have drastically changed dietary habits and lifestyles in the global south. As economies transition, more people are leading sedentary lifestyles, which have significant health consequences.
Trade liberalisation has increased the availability of cigarettes, alcohol, and highly processed foods—often heavily marketed by large multinational corporations. Their subsequent consumption has led to a rise in NCDs such as obesity, diabetes, and heart disease.
Demographics
Demographic changes, such as increasing life expectancy and declining fertility rates, have led to an aging population in many African countries. As people live longer, the prevalence of NCDs rises, further straining healthcare systems already struggling with limited resources.
The Inaction
The global surge of NCDs represents an unfolding health crisis in LMICs, but the response from the international community has been alarmingly insufficient.
Health system capacity is one of the key barriers to effective action. Skewed policy, programmes and investment mean that many health systems in Sub-Saharan Africa are built to focus on communicable diseases, which are largely easier to diagnose and have well-established treatment protocols. NCDs, on the other hand, often require more complex management, which becomes almost impossible without meaningful policy, programmes and investment.
NCDs were not part of the Millennium Development Goals and seemed to have missed out on funding opportunities during what was considered the ‘golden years’ of health funding despite causing more death and disability than any other disease group worldwide.
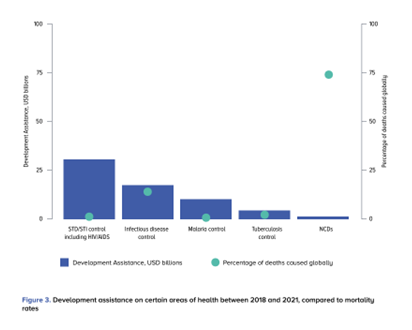
Figure 1: Development assistance on certain areas of health between 2018 and 2021, compared to mortality rates. (5)
The share of ‘development assistance for health’ dedicated to NCDs has remained at 1-2% of the total since 2000 (5). This level of funding is insufficient to attain the nine targets in the World Health Organization (WHO) Global Action Plan on NCDs. Diseases like HIV/AIDS, malaria, and tuberculosis still receive a disproportionate share of global health funding, despite causing fewer deaths than NCDs (figure 1) (1). This represents a massive failure of global funding institutions to acknowledge the real and changing health issues people are facing globally.
Without sufficient government or donor support, individuals often bear the full financial burden of managing chronic conditions, leading to devastating economic consequences for most.
What Can Be Done?
Rather than calling for a total reallocation of funds, reducing communicable disease capacity, there is a need for a broader approach to health funding—both in development assistance and in national budgets. Health systems must integrate NCD management with existing programmes, breaking down siloes that discourage cooperation and learning. Capacity building, advocacy, and prevention efforts are critical to reducing the burden of NCDs in LMICs. Governments, donors, and international organisations must ensure that essential care is accessible to everyone, particularly the most vulnerable, to address this growing crisis.
Community engagement and integrating NCD prevention into existing healthcare systems are essential to tackling the rise of diseases like cancer, diabetes, and heart disease. Involving community leaders, health workers, and those living with NCDs helps ensure interventions meet local needs, making care more accessible and relevant. This approach builds trust, reduces stigma, and encourages people to take preventive steps like regular screenings. Integrating NCD care into programmes like maternal health and HIV services is equally important, streamlining efforts and offering a more comprehensive and coordinated approach that addresses both health needs and underlying social factors.
Last year in partnership with Tropical Health & Education Trust (THET), we worked alongside health workers and communities in Ethiopia, we delivered essential education, screening and treatment to thousands of people to help tackle NCDs.

Woman getting her blood pressure checked in Afar, Ethiopia
Some of the key achievements of this intervention were (3):
- A total of 369,434 people were screened and 19,239 (5.2%) were diagnosed with an NCD. Among enrolled cases, hypertension was the most common diagnosis (74.4%) followed by diabetes (12.2%), chronic respiratory disease (9.3%) and epilepsy (4%).
- Trained 17 GPs and 208 nurses and health officers from project-supported health facilities to deliver quality diagnoses, treatment, and care to NCD patients.
- Trained 602 health extension workers on the risk factors, symptoms, and diagnosis of NCDs, and the referral systems.
- Almost 600,000 individuals were reached with health education on NCDs to improve health-seeking behaviour.
- Distributed a total of 25,000 copies of brochures and 1,000 posters across the target locations on NCDs, risk factors, and available services in nearby health facilities.
- A total of 237 mentorship and supportive supervisions were held to identify problems and challenges faced by health workers in their workplaces.
This was all possible with a simple programme, filling gaps in addressing NCDs within existing health systems. If you are interested in what this programme looked like and how we worked with both the Ministry of Health and communities to tackle the gaps in NCD care, you can read this article. We are investing our time and efforts into trying to increase the number of programmes where we can integrate NCD care.
References
1. Allen, L. N., 2017. Financing national non-communicable disease responses. Glob Health Action, 10(1).
2. Bigna, J. J. & Noubiap, J. J., 2019. The rising burden of non-communicable diseases in sub-Saharan Africa. The Lancet, 7(10), pp. 1295-1296.
3. Health Poverty Action; THET, 2023. Tenama Beteseb (Healthy Family) through decentralized NCD care in Ethiopia: Final Annual Impact Report , Addis Ababa, Ethiopia: Health Poverty Action; THET.
4. Ndubuisi, N. E., 2021. Noncommunicable Diseases Prevention In Low- and Middle-Income Countries: An Overview of Health in All Policies (HiAP). Inquiry, Jan-Dec(58).
5. The NCD Alliance; Global Alliance for Tobacco Control, 2024. Tracking NCD funding flows: Urgent calls and global solutions. [Online]
Available at: https://actonncds.org/sites/default/files/media/documents/Tracking%20NCD%20funding%20flows%20-%20Urgent%20calls%20%26%20global%20solutions_REPORT.pdf
6. WHO African Region, 2024. Noncommunicable Diseases. [Online]
Available at: https://www.afro.who.int/health-topics/noncommunicable-diseases#:~:text=In%20the%20WHO%20African%20Region%2C%20NCDs%20are%20increasingly%20becoming%20the,rising%20from%2024%25%20in%202000.

